











Unlike other mutation databases, HGMD mutations are backed by peer-reviewed publications where there is evidence of clinical impact—and the gold-standard, industry-leading resource just got better.
View the complete HGMD Professional statistics here.
When using Batch Search, the results table will now include a ClinVar column to the far right. This column will provide links to ClinVar records and list predicted classifications.


Read about the importance of having access to the most up-to-date and comprehensive database for human disease mutations in our white paper.
Learn how to take advantage of all HGMD’s features by watching our video tutorials available at our Resources Page.
New ANNOVAR databases are now available!
Learn more about how ANNOVAR can be used with HGMD for variant annotation.
Watch a recorded webinar featuring ANNOVAR here.
Genome Trax 2018.4 has updated tracks containing the 2018.4 HGMD release or all HGMD-related tracks.
Need a clinical genomic interpretation solution?
Look no further than QIAGEN Clinical Insight (QCI). Offering the highest level of interpretation transparency currently available on the market, QCI dynamically computes ACMG classification and AMP-tiering based on phenotype and clinical evidence. QCI incorporates knowledge from HGMD, CentoMD, over 30 public and proprietary databases, and over 2,000 scientific and clinical articles manually curated each month.
Kick start your year and sign-up for a free QCI demo here!
Though not technically summer, on May 25th, the EU passed the General Data Protection Regulation (GDPR) into law, creating a global ripple effect. The law impacts the world of clinical decision support software because it stipulates the “right to explanation,” around automated decision-making (i.e., algorithms) and the expected consequences of applying those decisions. This requirement for transparency does not bode well for the walled-off “black box” approach to clinical decision support. For another perspective, read this contributed piece in The Pathologist, written by our own Ramon Felciano, in which he positions QCI as an enabling tool to transition to precision medicine in a cost-effective, scalable, and transparent way.
Artificial intelligence (AI) was frequently in the news over the past few months. In particular, we saw quite a few stories about IBM’s Watson and its limitations in beating cancer. Though Watson has not yet lived up to its promise of generating insights and identifying new approaches to cancer treatment, there remains hope in the industry that AI will eventually revolutionize medicine—whether through data pattern recognition, its impact on pharmaceutical development, or—even someday—cancer. In the meantime, we at QIAGEN continue to focus on our clinical decision support tools (big data, informatics and augmented intelligence) to improve test interpretation and accuracy of results.
QIAGEN was in the news as well.
Our second consecutive win during AMP Europe’s Battle of the Bioinformatics Pipeline event was covered in GenomeWeb; we published our own recap of the results to provide additional detail and background around standardizing variant interpretation and reporting. Finally, we recently hosted three international OmicSoft User Group Meetings:
We hope you had a wonderful summer, and we look forward to the busier pace and renewed activity that fall brings.
Next-generation sequencing, bolstered by powerful data analytics and the clinical interpretation of genetic variants in a patient’s cancer, is on the cusp of transforming healthcare. We are at a watershed moment in medical history, comparable to the discovery of microorganisms, the development of vaccines, and the creation of antibiotics.
Precision medicine promises a paradigm shift in care delivery, one that removes the need for guesswork, variable diagnoses, and treatment strategies based on generalized demographics. Consider the tumor, for example. Once believed to be a uniform mass of malignancy, the tumor is now known to have tremendous genetic diversity, driven by a wide range of genetic mutations. Scientists continue to identify more and more of these mutations, which is crucial to the development of more targeted, and potentially much more effective, therapies. With therapies that go after mutations at the molecular level, there will inherently be better patient outcomes.
Yet, the progress of precision medicine now depends largely on getting data from discoveries into the hands of the doctors on the front lines of patient care. This is where QIAGEN Clinical Insight™ (QCI) is leading the way for predictive and preventative care. Below is a list of five trends shaping the precision medicine transformation and how QCI is tackling each challenge and opportunity.
Later-stage melanoma, colorectal, and lung cancer patients are now routinely offered DNA-based molecular diagnostic, theranostic, and prognostic tests. With the commonality of molecular diagnostic testing, numerous medical institutions are attempting to develop in-house testing capabilities. QCI enables molecular diagnostic labs and healthcare providers to develop and operationalize scalable, compliant, and secure molecular and genomic data analysis, interpretation, and reporting solutions to implement genomics-guided clinical decision support at the point of care.
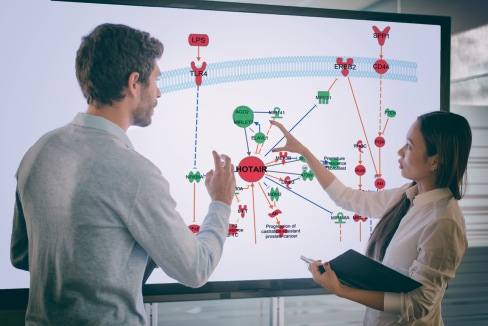
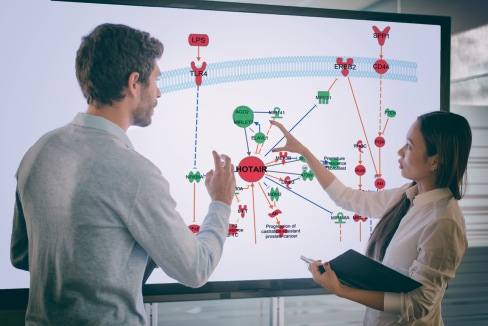
Understanding the differences in genomic results between different tumor profiling approaches will become increasingly important as the cancer genome is leveraged to stratify patients for new therapeutic strategies. However, the translation of results by community oncologists remains a major hurdle in the stratification of cancer into subtypes. A unique capability of QCI is the ability to recognize and interpret genetic factors that span multiple variants. Unlike alternative approaches that interpret a patient’s genetic profile on a variant-by-variant basis, QCI Interpret assesses the genetic profile in its entirety, matching combination variants that can influence the selection of an appropriate treatment or clinical trial.
Recent literature signals a growing paradigm shift toward integrating therapeutics and diagnostics, rather than developing them separately. In this gradual move toward more effective and personalized medications, “theranostics” is expected to increase response rates and improve patient outcomes. Yet, we continue to see variability in targeted therapy and trial matching. The QCI platform is a potent tool that evaluates genomic variants comparing them with published biomedical literature, professional association guidelines, publicly available databases and annotations, drug labels, and clinical trials. With QCI, clinicians will be able to rapidly classify variants, identify treatment options, and perform geographical clinical trial matching.
“Interpretation” remains the rate-limiting factor for the adoption and benefits of genomics-guided clinical decision support at the point of care; but, labs continue to invest a majority of their time and resources in instrument and assay selection. QCI shifts the focus from instrumentation to insight, catalyzing the rate of discovery and deployment of precision medicine capabilities. QIAGEN has developed the only publically available, industrial-scale, clinical-grade technology platform that can cost-effectively enable this capability for NGS testing laboratories. Thanks to an army of expert PhD curators, the QIAGEN Knowledge Base allows physicians and oncologists to develop patient-specific recommendations in the context of over 13 million relevant biomedical findings.
A recent U.S. Food and Drug Administration working group identified the need for improving standards of automated clinical NGS analysis, interpretation, and reporting policies. Widespread adoption of these guidelines will enhance communication between molecular pathologists, oncologists, and geneticists, as well as enhance patient care. QCI assists with the standardization of NGS analytical workflows by supporting virtually any clinical testing laboratory in developing and implementing a robust production pipeline for its cancer patient population.
Like nearly all aspects of healthcare, reaching the full potential of precision medicine will require collaboration among multiple players and a shift in current thinking: from information to insight. QCI is designed to fit into the clinical care workflow, which simplifies the adoption of precision medicine by delivering high-quality, scientific research to the bedside to improve patient care and outcomes.
By advancing the pace of precision medicine with QCI, any organization can harness the power of precision medicine to improve population health worldwide.
Learn more about QIAGEN Clinical Insight
Too much data and not enough biological meaning from your RNA-seq experiments?
What if you could:
• Save time with best in class analysis and streamlined statistics
• Achieve unique biological interpretation at the isoform level
• Identify potentially new causal connections between genes, or isoforms, and disease
Watch our webinar with Principal Scientist, Jean-Noel Billaud, Ph.D. and find out how to make sense of your results and publish faster.
Title: “Identification of potential immune targets in controlling Endometrioid Endometrial Carcinoma metastatic progression”
https://clcbio.23video.com/v.ihtml/player.html?token=2b7b885b45d7950598637f4b441d16bc&source=embed&photo%5fid=12956634
The February 2016 issue of Medical Lab Observer features a story co-authored by two QIAGEN Bioinformatics executives, Ramon Felciano and Michael Hadjisavas.
The story highlights the disparity between the increasing sophistication of genetic testing and the cumbersome process of variant analysis. It outlines a few key reasons for this growing gap, including the complexity of some variants, the traditional and painstaking process by which labs categorize variants, and the lack of consistency in reporting. The authors make the case that, to keep up with demand for genetic testing, the analysis piece of the puzzle needs to be fully automated, streamlined, and scalable. They call for a community-wide approach to overcome these challenges, such as the Allele Frequency Community. By sharing their resources, communities increase the value of the repository and not only help develop the market, but also improve patient diagnostics and care.
Check out the story: "Soaring demand for genetic testing highlights need for streamlined data interpretation". The article does a great job of addressing many key considerations regarding genetic testing interpretation, the resulting glut of data, and the increasing gap between the two. We hope you enjoy reading!
Read the full story
Read more about our products
It’s exciting to see that NGS-related bioinformatics advances are having an impact in clinical labs. We’ve been following that trend closely — so we are glad to read some excellent coverage of the topic recently in the highly regarded magazine CAP Today. We recap two of the articles here, and if you’d like you should of course give each of them a full read.
In “3 new NGS Surveys on CAP 2016 PT Launchpad,” author Anne Paxton highlights the overwhelmingly positive response to the College of American Pathologists’ (CAP) first proficiency testing for NGS. Some 130 labs participated, a far cry from the 35 labs CAP originally anticipated. This success prompted the group to expand its proficiency testing challenge to include bioinformatics in 2016, focusing first on molecular oncology and the detection of somatic mutations. CAP also expects to issue bioinformatics-based challenges in 2017 for germline variation and genetic disorders. In the story, Karl Voelkerding, chair of the CAP project team, says that the complexity inherent in NGS bioinformatics created a multitude of opportunities to organize, interpret, and deliver data.
An article from William Check entitled “Next-gen sequencing settling in, making its mark” touches on the increasing likelihood of finding NGS technology in labs at large health systems and hospitals (due in part to faster rates of reimbursement), as well as the reluctance of some clinical pathologists to embrace the technology. According to Check, technologies such as the Human Genome Mutation Database enable a strong evidence base when combined with high clinical utility. Her story is a testament to the value bioinformatics can bring to the clinical setting, particularly when testing can cover up to 500 genes in a single panel. The data produced by such testing is unwieldy, and requires a comprehensive bioinformatics solution to help clinicians identify the disease-causing variants that might otherwise have been missed. The author points out that many pathologists lack in-depth genomics or genetics training, which often creates a daunting obstacle for broader adoption of NGS technologies. He closes his story with practical pointers for pathologists to minimize their risk of being marginalized in this industry, where NGS and bioinformatics are playing an ever-increasing role.
Our team has spent many years developing expertise in content curation and genomic data analysis, and now we’re using that foundation to help clinical labs make quicker work of their data interpretation. We look forward to seeing how innovative bioinformatics approaches can make NGS-based testing more robust and reliable in the coming years.
Learn about QIAGEN Clinical Insight.