











The COVID-19 pandemic marked a turning point across the healthcare landscape. And like many professions, clincal cancer genetics is shifting in unexpected ways.
From changes to delivery models and the genetic testing landscape, to emerging new technologies and greater access, clinical genetics is at an inflection point. The demand for services is growing, patient cases are becoming more complex, and professional burnout is at an all-time high.
There’s a catalyzing culprit to these three challenges. Time. Across the industry, clinical geneticists and genetic counselors report time as the biggest bottleneck in their ability to provide services efficiently.
In a survey of cancer genetic counselors, 92% report not having enough time to properly prepare for new patient meetings.
This statistic gains greater impact when considering these five cause-and-effects:
Demand for clinical cancer genetics is soaring.
According to the U.S. Bureau of Labor Statistics, the field is projected to grow by 27% between 2018 and 2028, compared to just 5% across all professions.
Rapid growth in demand for clinical cancer genetics professionals has led to a workforce shortage.
There is approximately 1 clinical cancer genetics professional per 300,000 individuals in the United States (Pal et a. (2013)).
A workforce shortage places greater caseload pressure on genetic counselors.
According to the National Society of Genetic Counselors (NSGC) Professional Status Survey, 62% of clinical genetic counselors report an increase in patient volume in just two years (Patel et al. (2018)).
Case complexity is increasing.
A survey found that genetic counselors spend an average of 4-6 hours per patient working on case-prep, follow-up, and administrative tasks (Attard et al. (2018)).
Clinical geneticists are overwhelmed.
Up to three-quarters of clinical geneticists are found to be at moderate to high risk for burnout and compassion fatigue (Injeyan et al. 2011; Lee et al. 2015; Udipi et al. 2008).
Clinical geneticists and genetic counselors are experiencing compounded challenges. However, a closer look at a typical clinical cancer genetics workflow illuminates the main problem.
In a 2018 survey, 17 genetic counselors indicate that 64% of their time is spent on patient-related activities (PRA) versus face-to-face patient interaction. This equates to 3 hours of PRA time per patient. And, the most time-consuming part of the PRA was writing letters, which involves summarizing the genetic test results, providing detailed information, and recommending next steps—which all must be cited and supported by evidence.
Similarly, Heald et al. found that the most time-intensive part of a clinical geneticist’s and genetic counselor's workflow is literature review and exploring testing options. And, a recent study by Williams et al. found that clinical cancer genetics professionals spend an average of 420 minutes (7 hours) reviewing all available medical literature before presenting to physicians and their patients.
Clinical cancer geneticists and genetic counselors need a way to shorten the literature review process of their workflow without jeopardizing patient outcomes. They need a workflow that allows them to spend more time interacting with patients and less time behind a computer screen. They need a workflow that supports an increase in billing and reimbursement activities and decreases fatigue and burnout.
While some studies recommend improving efficiency by hiring a clinical genetics assistant—a “solution” that incurs substantial annual resources and costs—there’s an easier way forward.
The Human Somatic Mutation Database (HSMD) is the most time-efficient and cost-effective way cancer genetic counselors can scale caseload volume.
An easy-to-use, somatic database from QIAGEN, HSMD contains extensive genomic content relevant to solid tumors and hematological malignancies. Pulling content from over 419,000 real-world clinical oncology cases and 40+ databases contained in the QIAGEN Knowledge Base, HSMD gives genetic counselors access to over 1.5 million somatic variants characterized in over 1,400 cancer-related genes.
By incorporating HSMD into the workflow, clinical geneticists and genetic counselors can easily search and explore mutational characteristics across genes, synthesize key findings from drug labels, clinical trials, and professional guidelines, and receive detailed annotations for each observed variant.
Part of the reason clinical cancer genetics professionals are so willing to overwork is that they are uniformly compassionate people. You care deeply about your patients and want to do your best to help them through difficult times. As a result, these professionals are at high-risk for compassion fatigue.

A study published in Nature found that the primary reason why genetic counselors experience compassion fatigue is because you have to sometimes deliver “bad” news. Bad news could be a life-altering cancer diagnosis or the fact that there is not an available treatment for a specific patient.
When you incorporate HSMD into your workflow, you can be confident that you have considered every article and every therapeutic option that is known for a specific gene or variant. This gives you assurance that you are doing everything in your power to help your patients make informed decisions.
If you are a cancer clinical geneticist or genetic counselor that is experiencing an increase in caseload volume, under mounting pressure to meet with more patients, and feeling the stress of burnout and compassion fatigue, consider adopting HSMD into your workflow. QIAGEN Digital Insights offers free, no-obligation trials of the somatic mutation database. You can see what kind of content HSMD offers, explore the search functionality, and determine if this database can save you time and money.
Explore HSMD's features, content and applications with a free 5-day trial
REQUEST NOW
Today genetic innovation is advancing at breakneck pace. Since the first whole genome was sequenced in 2003, a feat that took 15 years, 20 different labs, and more than $3 billion to complete, a patient can now have his or her whole genome sequenced by one lab, in one day, for under $200.
Yet, only a fraction of patients receives genetic testing. Despite incredible advances in sequencing technology, most notable being next-generation sequencing (NGS), genetic has only recently become a clinical application. The challenge is no longer how to sequence DNA, but how to interpret a patient’s genetic variation in a meaningful and actionable way.
We are on the cusp of a healthcare revolution where genetic testing will be able to provide answers and insight into critical health questions. For a couple planning their family, genetic testing can identify carrier status. When a child has a rare condition with unexplainable symptoms, genetic testing can pinpoint a diagnosis. If a patient has a family history of cancer, genetic testing can predict the risk of developing disease.
A new reality is emerging in which genetic testing will transform our understanding and management of hereditary diseases. But before genetic testing becomes a routine part of clinical care for every patient, we must first address the complexity, cost, and consistency of NGS test interpretation.
Genetic disease is the leading cause of infant death in the United States, accounting for approximately 20% of annual infant mortality.1 Screening for genetic disease has been a long-established part of preconception and prenatal care, with a community wide screening program for Tay-Sachs disease (TSD) dating back to the 1970s; however, traditional methods of carrier screening have been offered gene-by-gene, disorder-by-disorder.
Recent developments in laboratory technologies have led to the commercial availability of expanded carrier screening (ECS) panels capable of assessing hundreds of mutations associated with genetic diseases. ECS panels have the ability to identify mutations that would otherwise not be detected. While many of the disorders on these panels are individually rare, the overall risk of having an affected offspring is 1 in 280, which is higher than the risk of having a child with a neural tube defect, for which screening is universal.2
In 2012, one of the first DNA testing and genetic counselling companies to offer ECS in the United States launched a flagship ECS panel that used next-generation sequencing (NGS) technology to assess thousands of mutations associated with more than 175 of the most relevant recessive diseases. For cancer-focused screens, the lab developed a 36 gene panel for hereditary cancer risk assessment.2
In the first three years of offering ECS, the lab screened over 400,000 individuals.3 By 2016, the lab served a network of more than 10,000 health professionals, and demand for preconception screening was soaring, owing to the increasing public awareness of the ill effects related to the transfer of genetic disease.4 Unique to the lab's ECS offering was the company’s “real-time manual curation” to support the classification of each genetic variant they encountered. Extremely thorough and highly accurate, the lab's manual literature curation enabled the company to elevate the actionable information provided to the ordering physicians and the patients they served. However, this process was labor-intensive and costly, which was ironic given the dwindling cost of DNA sequencing and the supporting technology. The question became how to scale-up without cutting corners.
Clinical decision support solutions have long been touted as the way of the future for clinical genetic testing laboratories. Combining big data analytics with advanced tools and knowledge bases, clinical decision support solutions are designed to organize, filter, and present useful information at the appropriate point in time to the person who can use it to make a decision. In 2017, the lab evaluated the use of a clinical decision support solution to help scale their genomic interpretation processes: QIAGEN Clinical Insight (QCI).*
QCI is QIAGEN’s clinical decision support solution for genetic testing laboratories. Software that reproducibly converts highly complex NGS data into clinician-ready reports, QCI is the tool through which actionable information is extracted from the sequencing results. Unlike any other clinical decision support solution on the market, QCI is largely powered by manual curation.
The knowledge base inside QCI is maintained by hundreds of Ph.D. scientists certified in clinical case curation who are committed to reading and recording all publications for a given mutation. This information is then mapped to over 2.8 million ontology classes contained within the QIAGEN Knowledge Base, providing further context by establishing relationships between variants, genes, tissue types, and pathways. When a genetic testing lab runs NGS data through QCI, the software computes the ACMG classification based on evidence curated from full-text articles, public, and private data sources. The knowledge extracted from full-text articles include observed genes, variants, function, phenotype, drug, dose, clinical cases, etc. With all this information stored in a structured knowledge base, the QIAGEN KB can quickly retrieve the relevant evidence that triggers all 28 ACMG criteria to more accurately compute an ACMG classification. Further this evidence is presented at the clinician’s fingertips for quick reference. Additionally, using natural language processing, the QIAGEN KB can auto-generate a one-sentence “finding” that is representative of the relevant evidence found in the published article.
This critical feature—automated curation of manually sourced content—saves genetic testing labs considerable time and effort when searching for variant-specific articles to satisfy the levels of evidence needed to definitively determine a classification. Especially for ECS, which is a testing practice that frequently encounters novel rare variants, the value of automation is fast becoming a necessity. To accurately and robustly appraise a novel rare variant’s pathogenicity, lab personnel must manually curate multiple lines of evidence to assess clinical significance. Therefore, if the majority of this information was autogenerated, the genomic interpretation process could be economically shortened.
The lab recognized the opportunity of integrating QCI into their curation workflow and designed a study to evaluate the concordance between the clinical evidence that QCI automatically retrieves for each observed variant classification and the clinical evidence that the lab’s curation team locates and ultimately uses in the physician reports. If the results were comparable, QCI could introduce significant time and cost savings.
The lab's manual curation workflow is outlined in Figure 1. A semi-automated process, the workflow utilizes proprietary software to initially classify variants into three categories: those with high population frequency; those that have never been reported; and those needing more information before pathogenicity can be assessed. For those remaining variants, the curation team manually searches online databases, in-house article libraries, and other available resources to find variant-specific references.
Figure 1. The lab's curation workflow
The curation workflow used to determine clinical significance of variants is summarized graphically. (a) The curation process is shown in the context of the overall laboratory workflow, in which inbound samples are eventually transformed into patient reports. (b) The curation workflow contributes lines of primary evidence that are reviewed manually, which are then combined with multiple lines of autogenerated supporting evidence to assess clinical significance.
Once evidence is collected for a variant —if any is to be found—the information is then used to assess the variant’s potential pathogenicity. As recommended by the American College of Medical Genetics (ACMG) and the Association for Molecular Pathology (AMP) published guidelines for the assessment of variants in genes associated with Mendelian diseases, the lab classifies variants following a two-step process:
First, the collected evidence is categorized into one of 28 defined criteria set forth by the ACMG-AMP guidelines and assigned a code that addresses the strength of evidence, such as population data, case-control analyses, functional data, computational predictions, allelic data, segregation studies, and de novo observations. Each code is assigned a weight (stand-alone, very strong, strong, moderate, or supporting) and direction (benign or pathogenic).
Next, the lab combines these evidence codes to arrive at one of five classifications: pathogenic (P), likely pathogenic (LP), variant of uncertain significance (VUS), likely benign (LB), or benign (B). Important in this step is the lab's ability to modify the strength of individual criteria based on expert discretion—a safeguard that goes away with computerized systems.
To determine whether QCI could provide value to the lab’s curation team, the software was tasked with pulling a bibliography for 2,324 variants that had been recently detected by the lab’s ECS and hereditary cancer risk assessment panels. For each of these variants, the curation team had been able to match at least one published article with a specific disease-gene reference. QCI’s variant bibliography was expected to present the same quantity and quality of clinical evidence.
The study found that QCI’s variant bibliography was highly concordant with lab’s manual curation efforts. Of the 2,324 unique article-variant pairs identified by the lab, QCI pulled 2,075 of the references (89.3%) and an additional 13,938 article-variant pairs not captured by the lab's curation team.
Figure 2. Overlap of bibliographic content
Figure 2 shows the overlap in content quantity between the two sources. As depicted, QCI (QIAGEN) presents significantly more data for the evaluated variants. This outcome reflects the comprehensive nature of QIAGEN’s article-centric approach, which aims to collect all publications for a given variant. While exhaustive and not always necessary, QCI’s ability to glean information from numerous sources affords the software greater accuracy in predicting variant classifications, which is seen in the second phase of the lab's evaluation.
More important than the number of bibliographic sources, accuracy of cited content ultimately dictates clinical significance. Counsyl measured the quality of QCI’s variant bibliography by looking at how the software would classify variants based on the information it pulled. What they found was a concordance of 98.8% of the pathogenic cases (Figure 2).
During the study period, a total of 682 variants were classified as pathogenic by lab’s genetic scientists. Of these, only eight would be downgraded to VUS utilizing only QCI bibliographies. Therefore, the false negative rate for using QCI’s bibliographies was ~1.2% and is expected to decrease to <1%. Further, for a sample of 50 VUS variants examined, none would change classification with additional unique references in QCI, primarily because QCI includes secondary reports and studies for other disease contexts that may be listed as 'reviewed but not curated' in their curations.
As a result of these positive findings, QCI bibliographies have been integrated into the lab’s manual curation workflow, eliminating the need for manual searches in the majority of cases. (Left: variant-specific page in QCI). After several months, a comparison of the time taken for reference searches before and after the adoption of QCI was performed (Figure 3).
Figure 3. Before and after adopting QCI
The goal of this evaluation was to assess whether utilization of QIAGEN’s variant-specific bibliographies could match the level of accuracy and quality of the lab’s more time-intensive manual article selection approach. Investigators concluded that there are clear benefits for adopting QCI for reference identification: an exceptionally high variant-specific article coverage, and significant time savings in a search process that can take up to ~45 minutes.
The results also serve to validate the efficacy of the lab’s previous article search and selection method, with the vast majority of variant classifications being unaltered by use of QIAGEN’s bibliographies. The lab now employs QCI bibliographies for every curated variant. Consequently, manual search methods are still employed at the lab, but can now be reserved for variants nearer VUS/pathogenic evidence thresholds.
QCI has already proven a valuable resource for increasing the efficiency of the lab’s in-house curation. Work is underway to additionally incorporate QIAGEN’s continually-updated bibliographies into the automated components of our variant classification workflows: the initial software-based auto-curation step for newly-identified variants, and the identification of those requiring re-curation in response to new publications becoming available. Accordingly, we expect QCI to further contribute to the lab’s continuing efforts to improve turnaround time by increasing curation efficiency while maintaining classification accuracy in patient reports.
*Data taken from a joint study conducted by Counsyl and QIAGEN: Cox et al. ClinGen 2017. Counsyl has since been acquired.
Learn more about QIAGEN Clinical Insight for here.
References
Structural variants affect large regions of the human genome and also play a significant role in gene expression (1, 2). They are typically detected with short Illumina or long PacBio reads, or a combination of both approaches. The new Advanced Structural Variant Detection (ASVD) plugin focuses on the short read approach, and is able to detect structural variants using short Illumina reads from whole genome sequencing (WGS). It supports the detection of the most frequently occurring structural variant types in the human genome such as deletions, duplications, and insertions (1).
The ASVD plugin checks read mappings for evidence of breakpoints using “unaligned end” signatures. “Unaligned end” refers to the end of a read that does not map to the reference sequence. At biological breakpoints, it is expected that multiple reads display unaligned ends, giving rise to a signature. A statistical model evaluates the likelihood of each breakpoint based on the probabilities of supporting reads. Breakpoint signatures and coverage information are next processed together in a series of steps. These include specialized alignment algorithms, copy number variation (CNV) detection, and local de novo assembly. If multiple structural variant calls are based on the set of breakpoints, the optimal calls given the breakpoint evidence are reported as the final set of detected structural variants.
Detected breakpoints and structural variants can be viewed together with the read mappings and the reference sequence. Track tables can then be used to filter and select individual breakpoints and structural variants as shown in the example in Figure 1.

Figure 1. Genome track view of the reference sequence, the read mapping of the sample and a track with the structural variant calls. The table view of the structural variant calls track allows interactive filtering and viewing of the results. An example of “unaligned ends”, i.e. ends of reads that do not match the reference genome, are seen as transparent ends of lines representing reads in the mapping.
To evaluate the performance of the ASVD plugin, we compared it to Illumina's Manta. Recent benchmarks against Delly and Lumpy showed that Manta had superior performance (3, 4).
We made use of two recent data sets from Huddleston et al. (5) and Shi et al. (6) to evaluate the ASVD plugin and Manta. Both of these studies used PacBio reads for contig assembly and structural variant detection concerning the GRCh38 reference.
While Shi et al. utilized a diploid genome from an anonymous Chinese individual HX1, Huddleston et al. sequenced two effectively haploid human genomes from hydatidiform moles CHM1 and CHM13 that hence lack allelic variations. Haploid genomes facilitate contig assembly and structural variant detection compared with diploid genomes, and we considered the CHM1 and CHM13 sets the most reliable truth sets available to our knowledge at the time of testing.
We combined the CHM1 and CHM13 sets to produce a diploid truth set, which contained 66.5% more calls than HX1. We believe this difference is mainly caused by the difficulty in detecting structural variants in a diploid genome, where Huddleston et al. showed that they were unable to recover the majority of their heterozygous calls when using an effectively diploid version of CHM1 and CHM13.
CHM1 and CHM13 Illumina reads were sampled to create three different sets of 20x, 40x, and 80x coverages, while the reads available for HX1 provided coverage of 75x. We note that our benchmarking method does not evaluate alternate but equivalent variant representations and that the truth set calls may not always be precise. We, therefore, used an error margin of 50 base pairs when comparing ASVD and Manta calls with structural variants in each truth set (see also special notes for further details regarding benchmarks and data preparation).
Table 1: Benchmark of ASVD and Manta on artificial diploid WGS reads at varying coverage, obtained by sampling form a mix of CHM1 and CHM13 reads in addition to a HX1 comparison. A SV was considered a true positive, if the call was within 50 bp of the truth.
| Dataset | Model | Correct | Wrong | Precision | Sensitivity |
| 20x | ASVD | 3561 | 355 | 0.909 | 0.109 |
| Manta | 2992 | 327 | 0.901 | 0.092 | |
| 40x | ASVD | 4896 | 520 | 0.904 | 0.150 |
| Manta | 4835 | 754 | 0.865 | 0.148 | |
| 80x | ASVD | 4924 | 582 | 0.894 | 0.151 |
| Manta | 6566 | 1242 | 0.840 | 0.201 | |
| HX1 (75x) | ASVD | 3398 | 2007 | 0.629 | 0.174 |
| Manta | 4230 | 2326 | 0.645 | 0.216 |
The ASVD plugin and Manta perform comparably across the different sets. Both the ASVD plugin and Manta showed significantly more “false positives” in the HX1 set compared with the Huddleston et al. 20x - 80x sets. We believe this is an artifact of real SVs that are present, but not included in the HX1 truth set.
We assessed the performance separately for short and long structural variants for the typical scenario of 40x coverage Illumina whole genome sequencing. A detailed comparison of results for the Huddleston et al. 40x coverage set in table 2, where we only considered variants of minimum 50 base pairs and applied a cut-off between short and long structural variants at 100 base pairs.
Table 2: Benchmark of ASVD and Manta for short and long structural variants for the 40x coverage Illumina data set. A SV was considered a true positive, if the call was within 50 bp of the truth.
| Length | Model | Correct | Wrong | Precision | Sensitivity | |
| Deletions | 50 – 100 | ASVD | 934 | 87 | 0.915 | 0.179 |
| Manta | 1084 | 203 | 0.842 | 0.208 | ||
| 100 – 10000 | ASVD | 2170 | 219 | 0.908 | 0.322 | |
| Manta | 2113 | 264 | 0.889 | 0.314 | ||
| Insertions | 50 – 100 | ASVD | 734 | 94 | 0.886 | 0.099 |
| Manta | 836 | 134 | 0.862 | 0.112 | ||
| 100 – 10000 | ASVD | 1058 | 120 | 0.898 | 0.081 | |
| Manta | 802 | 153 | 0.840 | 0.061 |
We observed instances where the ASVD plugin and Manta made equivalent calls that appeared correct, but were not present or were represented differently in a truth set. This resulted in lower precision and sensitivity values overall for both tools that is likely to be the case.
These benchmarks suggest that ASVD and Manta have very comparable performances for short SVs and that ASVD performs slightly better than Manta for longer CVs.
(1) Sudmant, P.H., et al. (2015) An integrated map of structural variation in 2,504 human genomes. Nature, 526
(2) Chiang, C., et al. (2017) The impact of structural variation on human gene expression. Nat. Genet. 49(5):692-699.
(3) Chen, X,., et al. (2016) Manta: rapid detection of structural variants and indels for germline and cancer sequencing applications, Bioinformatics. 32(8):1220-2.
(4) Sedlazeck F J., et al. (2018) Accurate detection of complex structural variations using single-molecule sequencing. Nat. Methods. 15(6):461-468.
(5) Huddleston, J., et al. (2017) Discovery and genotyping of structural variation from long-read haploid genome sequence data. Genome Res. 27(5):677-685.
(6) Shi et al. (2016) Long-read sequencing and de novo assembly of a Chinese genome. Nat. Comm. 30(7):12065.
Today, at the 60th Annual Meeting of the American Society of Hematology (ASH) in San Diego, California, QIAGEN announced the launch of two novel products to deliver actionable insights on a wide range of blood cancers: a new workflow for the QCI Interpret bioinformatics solution for hematological malignancies, and the new QIAact Myeloid DNA UMI Panel for use in myeloid neoplasm research as a Sample to Insight workflow on QIAGEN's GeneReader NGS System.

Meet and talk with our experts at ASH 18, booth #1557!
Featured Products and Solutions
Human Gene Mutation Database (HGMD®) is the gold standard industry-leading resource for comprehensive coverage of published human inherited disease mutations. Unlike other mutation databases, HGMD mutations are backed by peer-reviewed publications where there is evidence of clinical impact.
You can also prioritize variants by disease concepts via the drop-down menu.

You now have the ability to browse HGMD phenotypes mapped to the UMLS (grouped into disease concepts, e.g., blood disorders) during the phenotype search. You can also filter results using these disease concepts in batch search mode (see above).

To get the most out of your HGMD subscription, please watch the video tutorials available at our Resources webpage.
Learn more about how ANNOVAR can be used with HGMD for variant annotation.
Watch a recorded webinar featuring ANNOVAR here.
View the complete Genome Trax™ statistics
Updated tracks have been released concurrent with the HGMD release for all HGMD-related tracks. Additional major tracks updated include TRANSFAC® release 2018.3, PROTEOME™ release 2018.3.
The latest HGMD® Professional release is now available! Version 2018.2 contains a total of 232,443 mutation entries—that’s 7,801 more mutation entries than the previous release!
View the latest HGMD Professional statistics.
New HGMD Feature
References within mutation details now include the title of the cited journal articles.

As a reminder, HGMD Professional contains a significantly greater number of clinically relevant variants than ClinVar, OMIM, and SWISS-PROT, according to an analysis (Peterson et al., 2013),comparing variant mutation databases.

Read more about the importance of having access to the most up-to-date and comprehensive database for human disease mutations in our latest white paper.
ANNOVAR
A new version of ANNOVAR is now available! New features are listed below:
• Per user request, we have now made hg38 version of ensGene available through ANNOVAR
directly so that users do not need to build it themselves.
• avsnp150 is available through ANNOVAR now in hg19 and hg38 coordinate, to annotate your
variants with dbSNP identifiers.
• Latest clinvar (20170905) is available now through ANNOVAR in hg19 and hg38
coordinates. A long-standing problem on multi-allelic variants in ClinVar is now
addressed, so that multi-allelic variants are now correctly assigned to the corresponding
benign/pathogenic categories. The 20170130/20170501 versions are also updated to resolve
this issue.
• About 2.4 million Brazilian genomic variants with allele frequencies are available now in
hg19/hg38 coordinate. The data set comprises exomic variants of 609 elderly individuals
from a census-based sample from the city of São Paulo. Please use abraom as the keyword
to download and annotate, and refer to the original publication for details.
• pre-computed intervar scores (version 20180118) is available on both hg19 and hg38 now
with intervar_20180118 keyword. Only missense variants are included, and this is meant for
a quick-and-dirty analysis of most missense variants. For a more comprehensive/formal
calculation of scores, download https://github.com/WGLab/InterVar instead.
• Minor fixes and improvements.
Learn more about how ANNOVAR can be used with HGMD for variant annotation.
GENOME TRAX™
Updated tracks have been released with the HGMD release for all HGMD-related tracks. Additional major tracks updated include TRANSFAC® release 2018.2, PROTEOME™ release 2018.2.
Next-generation sequencing, bolstered by powerful data analytics and the clinical interpretation of genetic variants in a patient’s cancer, is on the cusp of transforming healthcare. We are at a watershed moment in medical history, comparable to the discovery of microorganisms, the development of vaccines, and the creation of antibiotics.
Precision medicine promises a paradigm shift in care delivery, one that removes the need for guesswork, variable diagnoses, and treatment strategies based on generalized demographics. Consider the tumor, for example. Once believed to be a uniform mass of malignancy, the tumor is now known to have tremendous genetic diversity, driven by a wide range of genetic mutations. Scientists continue to identify more and more of these mutations, which is crucial to the development of more targeted, and potentially much more effective, therapies. With therapies that go after mutations at the molecular level, there will inherently be better patient outcomes.
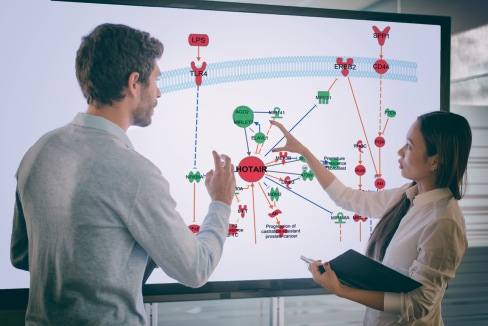
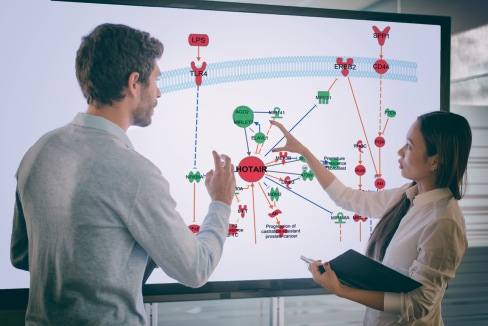
Yet, the progress of precision medicine now depends largely on getting data from discoveries into the hands of the doctors on the front lines of patient care. This is where QIAGEN Clinical Insight™ (QCI) is leading the way for predictive and preventative care. Below is a list of five trends shaping the precision medicine transformation and how QCI is tackling each challenge and opportunity.
Later-stage melanoma, colorectal, and lung cancer patients are now routinely offered DNA-based molecular diagnostic, theranostic, and prognostic tests. With the commonality of molecular diagnostic testing, numerous medical institutions are attempting to develop in-house testing capabilities. QCI enables molecular diagnostic labs and healthcare providers to develop and operationalize scalable, compliant, and secure molecular and genomic data analysis, interpretation, and reporting solutions to implement genomics-guided clinical decision support at the point of care.
Understanding the differences in genomic results between different tumor profiling approaches will become increasingly important as the cancer genome is leveraged to stratify patients for new therapeutic strategies. However, the translation of results by community oncologists remains a major hurdle in the stratification of cancer into subtypes. A unique capability of QCI is the ability to recognize and interpret genetic factors that span multiple variants. Unlike alternative approaches that interpret a patient’s genetic profile on a variant-by-variant basis, QCI Interpret assesses the genetic profile in its entirety, matching combination variants that can influence the selection of an appropriate treatment or clinical trial.
Recent literature signals a growing paradigm shift toward integrating therapeutics and diagnostics, rather than developing them separately. In this gradual move toward more effective and personalized medications, “theranostics” is expected to increase response rates and improve patient outcomes. Yet, we continue to see variability in targeted therapy and trial matching. The QCI platform is a potent tool that evaluates genomic variants comparing them with published biomedical literature, professional association guidelines, publicly available databases and annotations, drug labels, and clinical trials. With QCI, clinicians will be able to rapidly classify variants, identify treatment options, and perform geographical clinical trial matching.
“Interpretation” remains the rate-limiting factor for the adoption and benefits of genomics-guided clinical decision support at the point of care; but, labs continue to invest a majority of their time and resources in instrument and assay selection. QCI shifts the focus from instrumentation to insight, catalyzing the rate of discovery and deployment of precision medicine capabilities. QIAGEN has developed the only publically available, industrial-scale, clinical-grade technology platform that can cost-effectively enable this capability for NGS testing laboratories. Thanks to an army of expert PhD curators, the QIAGEN Knowledge Base allows physicians and oncologists to develop patient-specific recommendations in the context of over 13 million relevant biomedical findings.
A recent U.S. Food and Drug Administration working group identified the need for improving standards of automated clinical NGS analysis, interpretation, and reporting policies. Widespread adoption of these guidelines will enhance communication between molecular pathologists, oncologists, and geneticists, as well as enhance patient care. QCI assists with the standardization of NGS analytical workflows by supporting virtually any clinical testing laboratory in developing and implementing a robust production pipeline for its cancer patient population.
Like nearly all aspects of healthcare, reaching the full potential of precision medicine will require collaboration among multiple players and a shift in current thinking: from information to insight. QCI is designed to fit into the clinical care workflow, which simplifies the adoption of precision medicine by delivering high-quality, scientific research to the bedside to improve patient care and outcomes.
By advancing the pace of precision medicine with QCI, any organization can harness the power of precision medicine to improve population health worldwide.
Learn more about QIAGEN Clinical Insight
The next big medical frontier is on the horizon. Innovations in genomic technology are pushing us closer to the promise of precision medicine. It is remarkable to see how technological innovation has led to groundbreaking advances in genomics. In 2001, it cost nearly $3 billion to sequence the first human genome. Today, the price of whole-genome sequencing is around the $1,000 level, and in the figurative world of tomorrow, genome sequencing may be cheaper than a blood test. Indeed, the next ten years will witness a dramatic acceleration in the rate of discovery and the way in which healthcare is delivered will undergo an extraordinary transformation.
The April 2017 issue of Medical Lab Observer features an article written by QIAGEN Bioinformatics’ Chief Technology Officer Ramon Felciano, Ph.D. The article discusses the future of the genetic testing landscape over the next 10 years, highlighting the opportunities and challenges that the industry currently faces. From the development of robust data management systems, integration of genetic insights with new sources of health data, implementation of intelligent augmentation (IA) for data-driven decision support, and greater involvement of clinical lab personnel across the patient care continuum, genomics research holds the key to meeting many of the global healthcare challenges of the years ahead.
Check out the story: “Looking ahead: the future bioinformatics of genetic testing and precision medicine.” The article provides a thought-provoking outlook on how the next 10 years will usher in a new era of genomic medicine.
Discover how QIAGEN Bioinformatics is improving clinical decisions for cancer
We'll be joining Intel in their booth #2661 to share insights on NGS-based genetic testing across a range of cancer, hereditary, and rare diseases and you're welcome to stop by to learn more. We would also like to invite you to join the HIMSS17 Lunch & Learn: Enabling Precision Medicine Through NGS-based Screening and Diagnostic Testing
Monday, February 20, 2017, 11:15 am – 12:15 pm, Room 202A
Speakers
Ramon Felciano, CTO and Vice President,
Technology and Global Strategy Global Manager, Clinical Testing Solutions, QIAGEN Bioinformatics
And
Kristina Kermanshahche, Global Director Life Sciences, Intel
Our topics include NGS-based genetic testing across a range of cancer, hereditary, and rare diseases.
Learn how a leading academic hospital used a robust informatics platform to accelerate the deployment of validated precision medicine capabilities from sample to insight.
We (QIAGEN) provide an instrument-, platform-, assay- and pipeline-agnostic solution, that enables health care providers to scale sequencing, analysis, interpretation and reporting of screening, diagnostic and monitoring test offerings, fully integrated with hospital information systems.
Join the discussion on the importance of cost-effective and automated approaches for scaling an organizational capacity for analysis, classification and clinical reporting of relevant variants for delivery to physician providers.
Register online now to ensure a seat
If this is the first you've heard about HIMSS17 - which is the Health IT Conference 2017 - you can find more information on their website http://www.himssconference.org